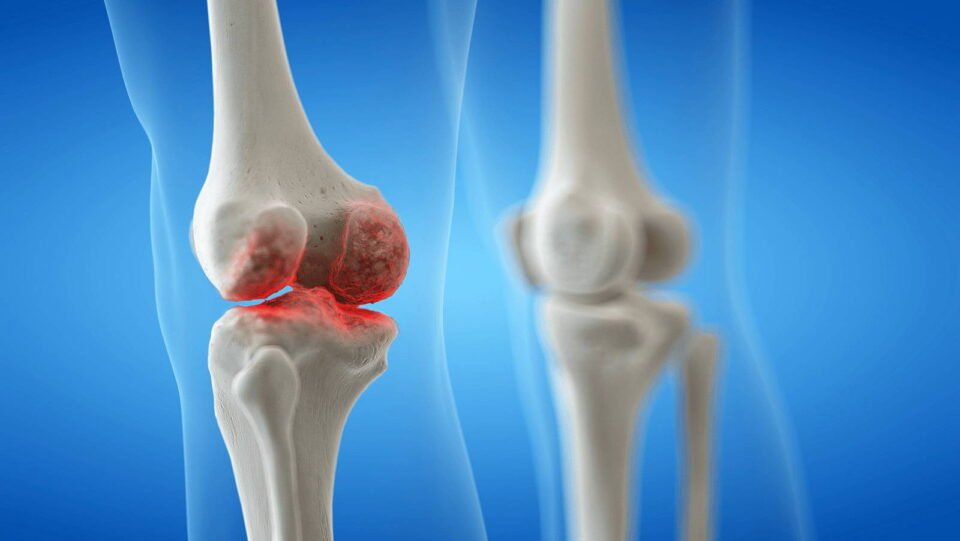
Knee joint infections, particularly following total knee arthroplasty (TKA), pose significant challenges for both patients and healthcare providers. These infections can lead to prolonged hospital stays, extensive antibiotic regimens, and multiple surgical interventions. Understanding the complexities involved in treatment is crucial for optimizing outcomes. The management of periprosthetic joint infections (PJIs) is multifaceted, requiring a careful assessment of various factors including patient health, infection type, and treatment options available. This blog explores ten critical considerations to keep in mind when addressing knee joint infection, ensuring a comprehensive approach to recovery.
1.Early Diagnosis is Key
Prompt identification of infection symptoms—such as swelling, pain, and fever—can significantly enhance treatment effectiveness. Diagnostic protocols should include synovial fluid analysis and imaging studies to confirm infection presence and guide management decisions.
2.Understanding Infection Types
Different pathogens involved in knee joint infections necessitate tailored treatment strategies due to their unique characteristics and resistance profiles. Gram-positive cocci, particularly are the most common culprits in these infections. Therefore, initial antibiotic therapy often focuses on these organisms, typically utilizing agents like vancomycin or daptomycin combined with a cephalosporin or fluoroquinolone to ensure effective coverage against these prevalent pathogens.
In contrast, Gram-negative bacteria and fungi may also contribute to knee joint infections, especially in patients with specific risk factors such as older age or immunosuppression. These pathogens might require broader-spectrum antibiotics to address the potential for resistance and the complexity of mixed infections. For instance, treatment for Gram-negative rods often includes agents that are effective against a variety of resistant strains. The presence of fungi may further complicate treatment, requiring antifungal agents alongside antibacterial therapy to achieve optimal outcomes.
Ultimately, the choice of antibiotic therapy should be guided by microbiological cultures and patient response to treatment. This individualized approach allows clinicians to adapt their strategies based on the specific pathogens identified and their susceptibility patterns, ensuring that patients receive the most effective care tailored to their unique infection profile.
3.Choosing the Right Treatment Strategy
The treatment options for knee joint infections, particularly periprosthetic joint infections (PJIs), vary significantly based on several critical factors, including the timing of the infection and the patient’s overall health. Two primary strategies are often considered: debridement with implant retention and two-stage revision arthroplasty. Debridement and implant retention, known as DAIR, is typically employed for early infections, particularly within four weeks of surgery. This approach involves thorough surgical cleaning of the infected tissue while retaining the original implant, provided it remains well-fixed and functional. DAIR is advantageous due to its lower morbidity and quicker recovery compared to more invasive procedures.
In contrast, two-stage revision arthroplasty is often regarded as the gold standard for treating established infections, especially those occurring later than four weeks post-surgery. This method involves first removing the infected implant and placing an antibiotic-loaded spacer to control the infection before a second surgery is performed to re-implant a new prosthesis. While this approach may entail longer recovery times and more extensive rehabilitation, it has demonstrated higher success rates in eradicating infections.
Ultimately, the choice between these treatment strategies should be individualized, taking into account factors such as the virulence of the infecting organism, patient age, comorbidities, and preferences. A thorough evaluation by a multidisciplinary team can ensure that the selected treatment aligns with the patient’s specific needs and maximizes the chances of successful recovery.
4.Antibiotic Therapy Duration
The duration of antibiotic therapy typically spans from two to six weeks, depending on the infection’s severity and response to initial treatments. Continuous monitoring is essential to adjust therapy as needed.
5.Surgical Interventions
Surgical options may include debridement with implant retention (DAIR) or staged revisions. Two-stage procedures often yield higher success rates but involve longer recovery times due to the use of antibiotic spacers.
6.Patient Factors Matter
Individual patient characteristics—like comorbidities and immune status—play a crucial role in treatment success. A thorough assessment helps tailor interventions that align with the patient’s unique situation.
7.Importance of Multidisciplinary Care
Effective management of knee joint infections, particularly periprosthetic joint infections (PJIs), necessitates a collaborative approach involving orthopedic surgeons, infectious disease specialists, and rehabilitation teams. Each discipline contributes unique expertise essential for comprehensive care. Orthopedic surgeons are primarily responsible for the surgical interventions required to manage the infection, whether through debridement or revision arthroplasty. Their skills are crucial in assessing the integrity of the implant and determining the most appropriate surgical strategy based on infection timing and severity.
Infectious disease specialists play a pivotal role in guiding antibiotic therapy. They evaluate the specific pathogens involved, recommend appropriate empirical treatment, and adjust antibiotic regimens based on culture results and sensitivity patterns. This collaboration ensures that patients receive targeted therapy that addresses the unique challenges posed by different infectious agents. The integration of their expertise is vital for managing complex cases where antibiotic resistance may complicate treatment.
Rehabilitation teams are equally important in the recovery process. They focus on restoring function and mobility post-surgery, which is critical for improving patient outcomes. Early rehabilitation can mitigate complications such as stiffness and muscle atrophy, enhancing overall recovery. By fostering an interdisciplinary approach, healthcare providers can ensure that all aspects of patient care are addressed, leading to better outcomes in managing knee joint infections.
8.Monitoring for Complications
Regular follow-ups are necessary to monitor for potential complications such as recurrent infections or joint stiffness, which can impact long-term outcomes.
9.Rehabilitation Considerations
Post-treatment rehabilitation should begin as soon as feasible to restore function and mobility while minimizing stiffness. Early intervention can significantly improve recovery trajectories.
10.Patient Education and Engagement
Informing patients about their condition, treatment options, and expected outcomes fosters better engagement in their care process. Empowered patients are more likely to adhere to treatment plans and participate actively in their recovery.
In conclusion, joint infection treatment requires a nuanced understanding of various factors influencing outcomes. By considering these ten essential aspects, healthcare providers can enhance their approach to managing PJIs effectively, ultimately improving recovery rates and patient satisfaction.